The development of the fetal cardiac system is a marvel of nature, intricately timed, and essential for the growing embryo. By day 21 post-fertilization, the heart initiates its rhythmic beats, establishing circulation patterns crucial for supplying gases and nutrients to the fetus, while also eliminating waste. This blog post delves into the remarkable progression of the fetal cardiac system and the critical considerations when medications are part of a perinatal treatment plan.
Embryonic Cardiovascular Development
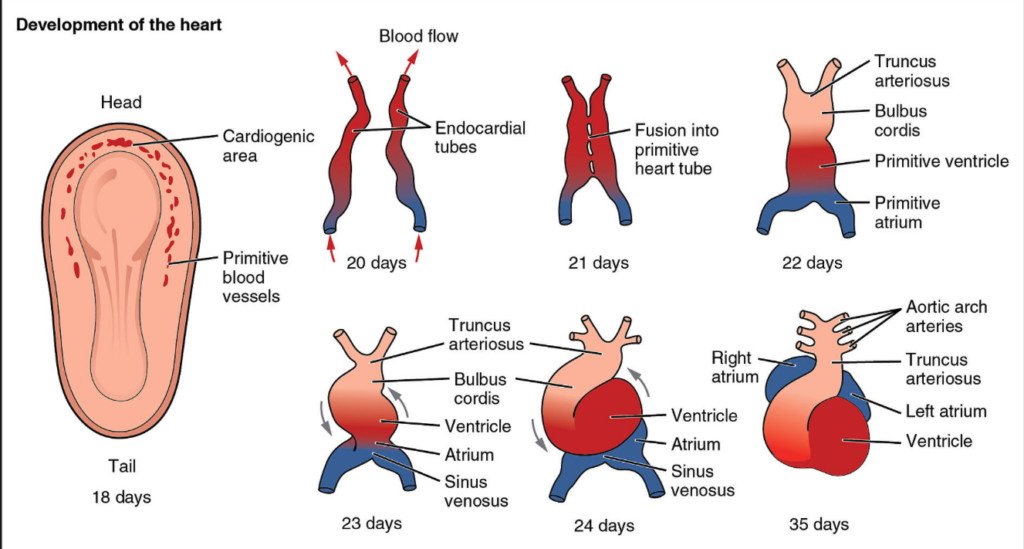
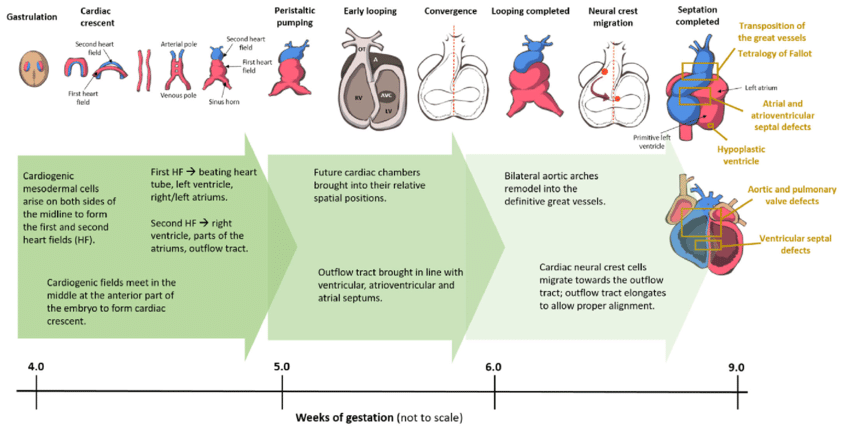
Around the third week of embryonic development, the heart tube originates from mesodermal cells. It elongates and undergoes looping, giving rise to the basic structure of the heart.
By the end of the fourth week, the heart tube begins to differentiate into distinct chambers, including 2 atria and 1 ventricle.
Septation then occurs, which divides the primitive heart into 4 chambers, 2 atria and 2 ventricles.
Valves form to ensure unidirectional blood flow between the chambers.
Then the conduction system of the heart, include the SA and AV nodes, and bundle of His, begins to form. These structures are essential for the rhythmic contractions of the heart.
As the heart further develops, it connects to the circulatory system by forming connections with major blood vessels.
Development of the embryo progresses and by the 10th week of gestation, the fetal circulation undergoes a transformative shift. The fetal circulation transitions from a passive gas exchange to a placenta dominant system.
Navigating Medication Considerations
The journey of fetal cardiac development intertwines with the intricate decisions pregnant individuals face regarding medication use, especially when managing mental health conditions. Here, we’ll explore specific considerations for lithium, stimulants, and antidepressants used in pregnancy.
Lithium and Bipolar Disorder
For individuals managing bipolar disorder with lithium, careful consideration is paramount. Discontinuation of medication poses a high risk of recurrence throughout pregnancy and the postpartum period. Women who discontinue the use of medication during pregnancy have roughly an 85% risk of relapse. Conversely, women who maintain medication management have a 37% chance of relapse. Additionally, untreated bipolar disorder increases the risk of prematurity and small for gestational age babies. Postpartum psychosis is a serious mental health illness that affects roughly 1 in 1,000 mothers after giving birth and is linked in many cases to an underlying bipolar disorder.
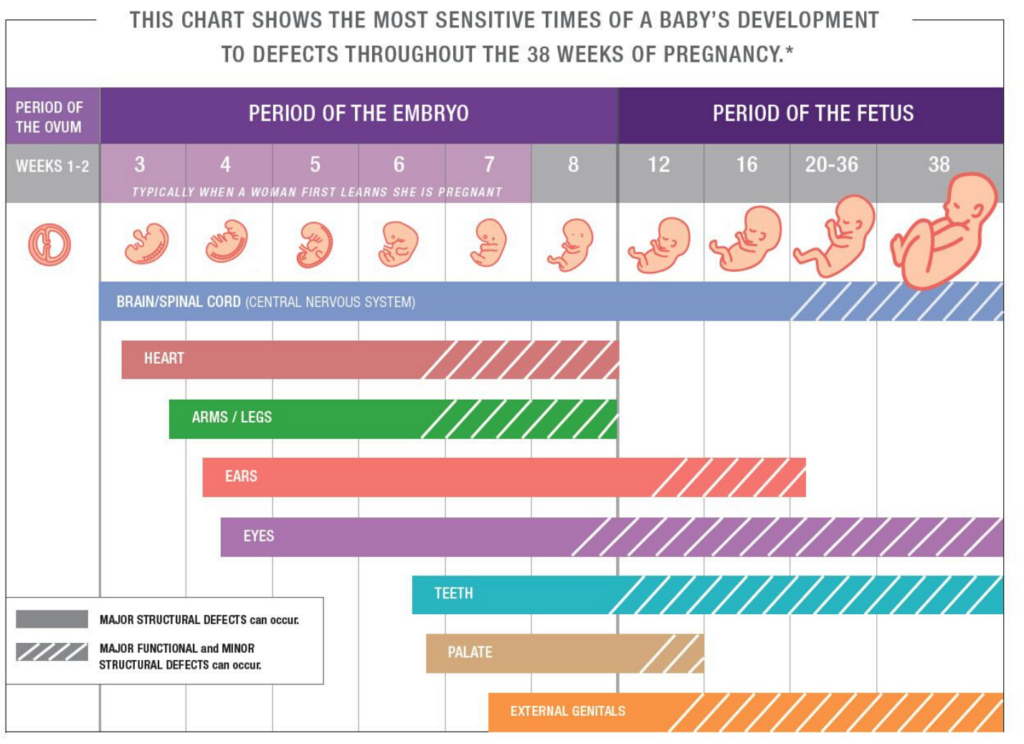
Lithium use during pregnancy presents a small but statistically significant increased risk for cardiovascular malformations. Ebstein’s anomaly is the most common cardiac defect associated with lithium use, and is characterized by abnormal development of the tricuspid valve and displacement of the valve leaflets into the right ventricle. This can lead to backflow of blood from the right venticle to the right atrium and lead to decreased efficiency of the heart. Cases can be mild without significant symptomatology, or more severe and requiring surgery. Compared to women with no medication exposures, the relative risk of cardiac malformations for lithium exposure is about 1.65. There is also thought to be a dose relationship, where risk increases significantly for doses of lithium over 900 mg daily. The bottom line is that lithium carries some teratogenic risk, though increased risk is fairly low at doses below 900 mg daily. To monitor this risk, women treated with lithium during pregnancy typically undergo a fetal echocardiogram.
Stimulants in Pregnancy
While women with mild-moderate ADHD may opt for non-pharmacologic management during pregnancy, women with moderate-severe ADHD often require continued stimulant treatment to maintain occupational and social functioning and to minimize safety risks. While the older data on stimulants, often examined in a population using these medications abusively, was concerning for cardiac malformations and decreased fetal growth, the newer studies we have are much more reassuring.
Newer studies do not show any increased risk for congenital malformations with use of amphetamines during pregnancy, though there is s small increased risk for cardiac malformations in methylphenidate exposed children. I do recommend careful blood pressure monitoring through pregnancy, and especially if on a stimulant, as these medications can contribute to risk for gestational hypertension.
Antidepressants and Maternal Mental Health
Antidepressants, commonly used to manage depression and anxiety during the perinatal period, have overwhelming reassuring data during the perinatal period. Selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants, are not thought to increase the risk of cardiac malformations. Early reports did suggest a link between cardiac septal defects and exposure to paroxetine, though more recent studies do not support this association.
Data on the reproductive safety of buproprion is generally reassuring, but more limited than the data we have for the SSRI/SNRI medication. There have been several studies showing an increased risk for cardiovascular defects with buproprion, through absolute risk is small. There are other studies that do not show any association between buproprion and cardiac defects. Some positive studies may be confounded by the smoking cessation indication for buproprion. While overall studies are mixed, if there is any increased risk, it is thought to be small.
Strive to Make an Intentional Decision
With any medication decision during the perinatal period, we must consider both fetal risk as well as maternal mental health. Every decision is framed as a risk-risk analysis, with the goal of choosing the side of less overall risk, acknowledging that no choice is completely risk free. It is essential to understand the timeline of fetal cardiac development and the medications that can present cardiac risks to the fetus so you can make the most informed choice about your medication plan during this period.